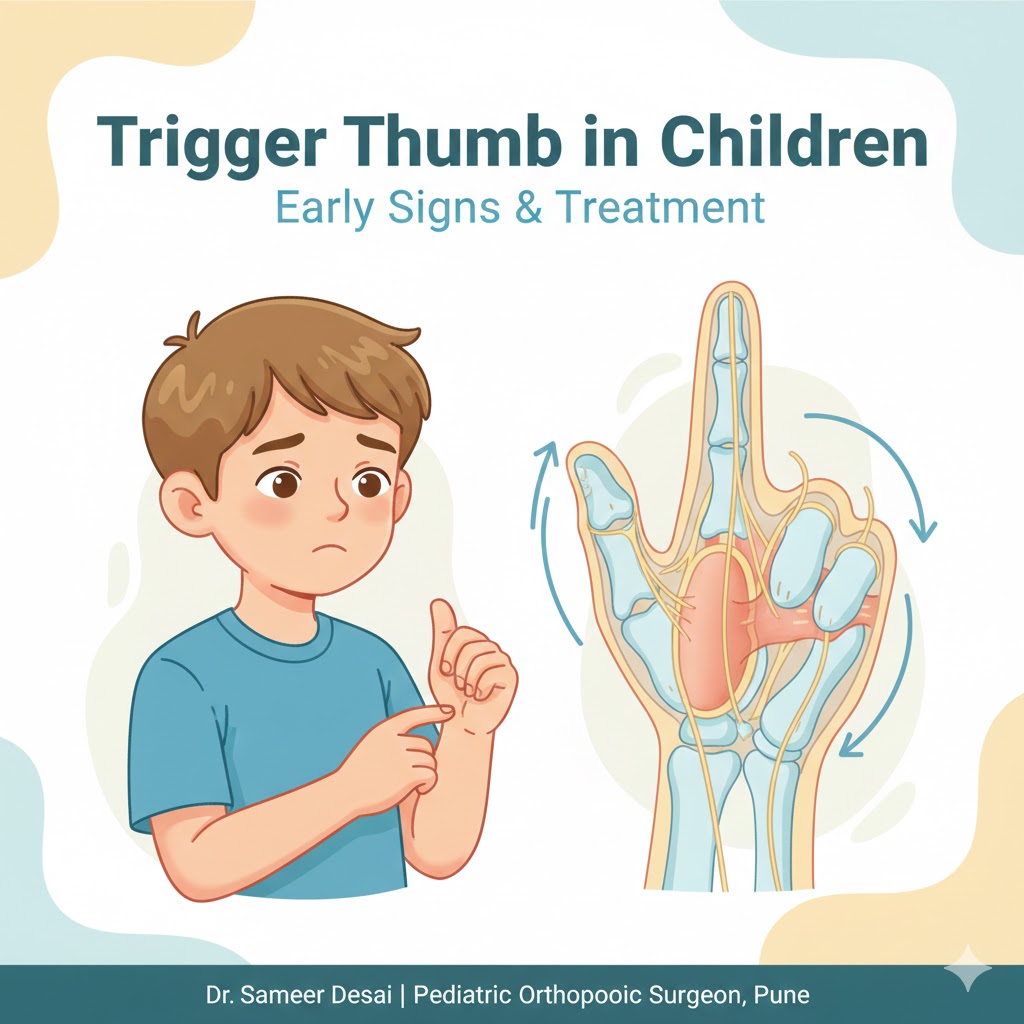
Trigger Thumb in Children: Early Signs, Causes & Effective Treatment in Pune
Parents often notice small changes in their child’s hands before realizing something may be wrong—like a thumb that doesn’t straighten fully or makes a clicking sound while moving. This condition is commonly known as Triger Thumb, and when treated early, children can regain completely normal hand function. If you’re looking for expert care, Dr. Sameer Desai, a trusted pediatric orthopedic surgeon in Aundh, Pune, specializes in diagnosing and treating trigger thumb and other orthopedic conditions in children. What Is Trigger Thumb in Children? Trigger thumb occurs when the tendon responsible for bending the thumb becomes thickened or inflamed. This makes it difficult for the tendon to glide smoothly, causing the thumb to lock, bend, or click during movement. Unlike adults, children may not complain of pain. Instead, parents often notice stiffness or an unusual position of the thumb. Common Symptoms of Trigger Thumb Children with trigger thumb may show one or more of the following signs: Thumb stuck in a bent position Clicking or popping sound while moving the thumb Stiffness, especially after sleep Tenderness or a small lump at the base of the thumb Difficulty straightening the thumb without help Early evaluation by a Child Orthopedic Surgeon in Pune is important to prevent long-term stiffness. Why Does Trigger Thumb Occur in Kids? The exact cause is not always known, but possible reasons include: Thickening of the tendon sheath Congenital tendon tightness Repetitive thumb movements Minor inflammation over time The good news is that it is highly treatable, especially when diagnosed early. Trigger Thumb Treatment in Pune Treatment depends on the child’s age and severity of the condition. Non-Surgical Options (Early Stages): Gentle stretching exercises Observation and regular follow-ups Splinting in selected cases Surgical Treatment (When Needed): If the thumb remains locked or stiff, a minor surgical release may be advised. The procedure is quick, safe, and has excellent outcomes when performed by an experienced Pediatric Orthopedic Surgeon in Pune. Dr. Sameer Desai is known for using child-friendly, minimally invasive techniques that ensure faster recovery and minimal discomfort. Why Choose Dr. Sameer Desai? Highly experienced Pediatric Orthopedic Surgeon in Aundh, Pune Specialized care for trigger thumb, clubfoot, knock knees & limb deformities Child-focused approach with gentle treatment planning Trusted name for Trigger Thumb Treatment in Pune When Should Parents Consult a Specialist? If your child’s thumb: Remains bent for weeks Makes clicking sounds Does not straighten naturally It’s best to consult a Child Orthopedic Surgeon in Pune without delay. Book Expert Pediatric Orthopedic Care in Pune For accurate diagnosis and advanced care, consult: Dr. Sameer Desai | Pediatric Orthopedic Surgeon in Aundh, Pune | Clubfoot | Knock Knees | Pediatric Orthopedic Early treatment ensures normal growth, movement, and a pain-free future for your child.
Trigger Thumb in Children: Early Signs, Causes & Effective Treatment in Pune Read More »